Gastroparesis is a health problem that impacts the usual functioning of stomach muscles. It causes slow gastric emptying, so food stays in the stomach longer before moving to the small intestine. This issue could be due to different reasons such as damage to nerves, especially the vagus nerve that regulates muscles in our stomach. The precise reason is frequently uncertain, however, conditions such as diabetes, surgical procedures, and specific medicines can lead to the formation of gastroparesis. Comprehension of gastroparesis becomes necessary for recognizing its signs and investigating treatment possibilities for efficient control.
Recognizing Gastroparesis Symptoms
People who have gastroparesis might feel different symptoms that can greatly change their everyday life. Usual signs are feeling sick, throwing up, feeling bloated, and early fullness where people sense they are filled just after eating a little bit of food. They may also feel pain in the belly area and lose weight because they eat less. Certain individuals might notice changes in their sugar levels in the blood, especially those who have diabetes. This could be due to delayed emptying of the stomach which can affect how glucose gets absorbed. Knowing these signs is very important as it leads one to look for suitable medical guidance and help. It's because these symptoms may resemble other issues related to the digestive system, hence making the identification quite tough.
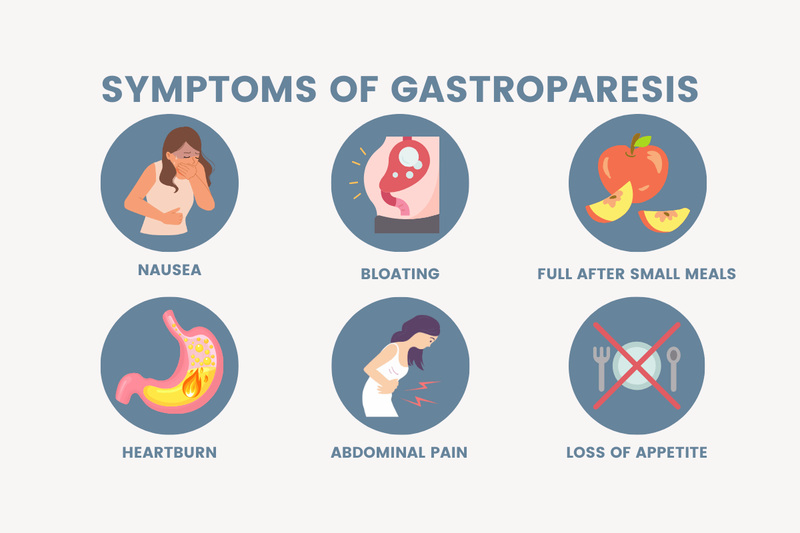
Besides the normally identified signs, some people can also have heartburn and gastroesophageal reflux which make their medical situation more difficult. The presence of stress or anxiety might make these symptoms worse, creating a pattern that impacts overall health. Knowing about these extra elements could assist patients in having better communication with their healthcare givers and may result in more custom-made treatment plans.
- Fluctuation in Symptoms: Symptoms can vary in intensity over time, influenced by diet, stress, and physical activity levels.
- Emotional Impact: The chronic nature of gastroparesis can lead to feelings of frustration and depression, making psychological support crucial.
Diagnosis and Tests for Gastroparesis
Usually, to find out if someone has gastroparesis, a careful check of their symptoms and past health conditions is done. Medical professionals can do different tests to see how food moves in the stomach. A usual test involves patients eating a meal with little radioactive matter which is called a gastric emptying study. Pictures are captured in some hours to monitor the speed of food leaving the stomach. More methods for diagnosis can be using ultrasound or upper gastrointestinal endoscopy to dismiss other diseases. It is very important to determine a correct diagnosis so that efficient treatment plans, that suit patients' unique needs, can be put into effect.
Besides the gastric emptying study, medical professionals might use other ways like the breath test. This test checks how well the body digests certain foods. They can also do an endoscopy to understand the stomach's structure and find if there is any physical blockage. Going through a full diagnostic process makes sure that no hidden conditions are missed which leads to more focused treatment plans.
- Comprehensive Evaluation: A multidisciplinary team approach may be beneficial, involving gastroenterologists and dietitians to ensure all aspects of the patient's health are addressed.
- Regular Monitoring: Routine follow-up assessments are important to track the progression of symptoms and the effectiveness of the treatment plan.
Treatment for Gastroparesis
Handling gastroparesis usually needs a complex strategy, which tackles both symptoms and root causes. The treatment for this condition may call for alterations in diet, use of medicines, and adjustments to daily routines. Doctors might suggest eating smaller portions but more often that have less fat and fiber content because these types of food are simpler to digest. Drugs like prokinetics can aid in boosting muscle contractions of the stomach and enhancing digestion. Moreover, anti-sickness drugs might be given to ease discomfort. In circumstances where there's no response to regular treatments and the condition is grave, more developed solutions such as gastric electrical stimulation or even operation could be contemplated.
With medicine and changes in eating habits, patients can find great improvements by altering their life routines. Physical activity often helps digestion and boosts overall health. Added to that, patients need to keep talking with those who provide healthcare services about any difference in symptoms as this may mean a need for change in treatment plans.
- Medication Compliance: Adhering to prescribed medication schedules is crucial for maintaining symptom control and preventing complications.
- Lifestyle Factors: Reducing caffeine and alcohol intake may enhance treatment effectiveness, as these substances can irritate the digestive tract.
Managing Gastroparesis Diet

Nutrition is very important in managing gastroparesis. A properly planned nutrition can reduce symptoms and make life better. People are usually recommended to have smaller meals many times a day instead of three big ones because it helps not overload the stomach. Food that is easy to digest like cooked vegetables, proteins with, low fat, and carbohydrates with less fiber is often suggested. It is critical not to eat foods high in fats or fiber as it can worsen the slow stomach-emptying process. Also important is keeping the body hydrated but drinking fluids between meals rather than during may help improve digestion better. Maintaining a record of food can aid people in recognizing which foods provoke symptoms and modifying their diet as needed.
Moreover, thinking about the ways of preparing food can improve its ability to be digested. Cooking techniques like steaming, baking, or poaching are often more liked because they keep nutrients in the foods and make them easier for digestion. It is also very important to know portion sizes since smaller amounts can stop feelings of being full and discomfort which allows for improved intake of nutrition.
- Nutrient Monitoring: Tracking daily intake of essential nutrients can help ensure that dietary modifications do not lead to deficiencies.
- Personalized Adjustments: Each patient's response to foods can differ; therefore, personalized dietary recommendations are beneficial for effective management.
Coping Strategies and Support for Gastroparesis
To dwell with gastroparesis might turn out tough, in both body and mind aspects. It's a must for those suffering to possess firm support circles like medical caregivers, family members, and friends assisting them handle this situation. Becoming part of some supportive groups or obtaining guidance could offer emotional comfort along with useful suggestions from people who comprehend the hardships associated with controlling gastroparesis. Often, it is of great help to have continuous meetings with health experts for condition assessment and required modifications to the medical plan. More so, knowing their illness gives individuals power over their well-being, resulting in improved methods of management.
It's very important to find ways to deal with the emotional stress that often accompanies long-term sickness. Activities like mindfulness and yoga can be beneficial in reducing anxiety, they also help improve emotional strength. In addition, participating in support groups where experiences are shared helps create a feeling of belonging and comprehension; this allows patients not to feel alone when facing their health challenges.
- Resource Utilization: Leveraging online resources, such as educational websites and forums, can provide additional information and support for patients.
- Family Involvement: Encouraging family members to learn about gastroparesis can enhance emotional support and improve communication within the household.
Conclusion
Gastroparesis is a complicated condition that needs deep understanding to manage it effectively. Identifying the symptoms and getting a quick diagnosis are important steps in handling issues caused by this illness. Different ways of treatment like changing food habits, using medicines, and altering lifestyle can greatly enhance the quality for people suffering from it. People must stay active in controlling their health, working together with healthcare experts, and using the support systems accessible. Living with gastroparesis might be tough but through the right management, they can understand it better which could enhance general wellness.







